IVF treatment and process
What is in vitro fertilisation (IVF)?
In vitro fertilisation (IVF) is a process where sperm fertilises the eggs in the laboratory (rather than in the woman’s fallopian tube). This involves:
- Placing the egg from the woman together with many thousands of sperm (typically 100,000).
- The fertilised embryos grow in the laboratory over five days (blastocyst stage) before being transferred into the woman’s uterus in a simple procedure called embryo transfer.
- The embryo transfer process involves passing a very fine tube containing the embryo through the cervix and into the uterine cavity. Usually one embryo at a time is transferred with additional embryos stored by freezing for use in subsequent treatments.
Enquire Today
Who is IVF suitable for?
For many couples or individuals in vitro fertilisation (IVF) offers the best chance of achieving a pregnancy. IVF treatment may be recommended in a range of conditions affecting fertility, including sperm abnormalities, endometriosis, tubal damage, unsuccessful ovulation induction and unexplained infertility. IVF may also be an option for single women and same-sex and gender diverse couples who choose to use donor sperm to have a baby.
If the sperm profile is poor the process of fertilisation is carried out by intracytoplasmic sperm injection (ICSI), where a single sperm is injected into each egg. Fertilisation then takes place over a number of hours in a culture dish maintained under ideal conditions in the laboratory.
Learn about our leading scientists who direct the tasks associated with an IVF cycle »
What is my chance of IVF success?
The success rate of IVF can vary widely and is mostly influenced by the age of the female partner. Visit our success rates page for a breakdown of IVF success rates by age group.
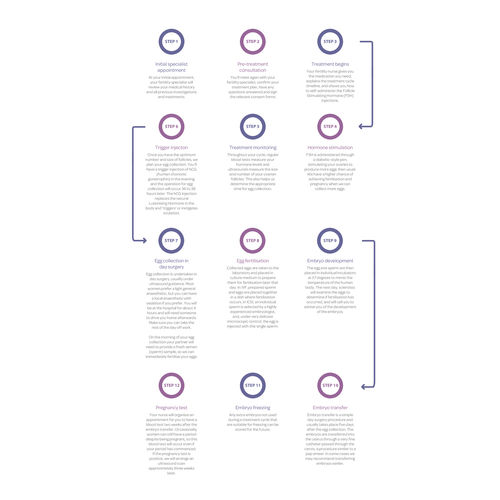
The IVF process step by step
The active phase of an IVF treatment takes place in the first two weeks of a cycle and involves a number of steps. Here we explain what happens in a typical IVF cycle:
Step 1: Fertility Specialist Appointment
At your consultation with your Fertility Specialist your medical history will be reviewed, any initial tests ordered and initial advice provided. Based on the results of the initial tests, a treatment plan will be recommended. Should your doctor recommend IVF he or she will explain the IVF process. The following points outlined in this IVF process step by step diagram will help you understand the IVF process timeline. This diagram relates to a typical IVF treatment cycle, known as the down regulation IVF treatment cycle, one of the most common treatment protocols for patients commencing IVF treatment.
For patients accessing genetic testing or PGT treatment cycles, review the PGD process here.
Step 2: New Patient Appointments
As a new patient, you can visit the Patient Liaison Administration (PLA) team in person, or alternatively your PLA will contact you to arrange your new patient appointments.
These appointments can be organised over the phone or face to face, and include:
- A counselling appointment
- A new patient appointment with a nurse; and a
- Patient Liaison Administration appointment
Step 3: New patient information session with a nurse
Attend a new patient information session with a nurse who will explain the IVF treatment process with you, including any specific treatment ordered for you by your fertility specialist as part of your IVF treatment. They will teach you how to administer the injections and medications, and discuss the IVF process timeline with you.
Step 4: Patient Liaison Administrator appointment
Attend an appointment with a PLA to explain the IVF treatment costs, discuss your payment options and any potential Medicare rebates, and answer any questions that may arise.
Step 5: Mandatory counselling session
Attend a mandatory counselling session with both partners, to assist in considering any issues that may arise throughout upcoming treatment and to sign mandatory consent forms. The counsellor will explain the supportive counselling available to you during your treatment, as well as help you prepare psychologically and emotionally for treatment.
Step 6: Preparing for treatment
Once you have made the decision to proceed with IVF treatment, it is really important that you call the Patient Liaison Administration team on the first day of your period, to organise payment, ensure that you are ready to start treatment, check your Medicare details so that you can access rebates (if eligible), and confirm your preferred payment option. The Patient Liaison Administrator will organise for you to speak with a member of your nursing team, who will co-ordinate your treatment.
Step 7: Treatment Begins
To commence your IVF treatment, call your PLA to advise of day 1 of your period. Your PLA will then transfer you to the nurses. The nurses will then coordinate the dates of the remainder of your IVF treatment plan.
Step 8: Down regulation medication begins (used on a case by case basis)
Down regulation medication is used to suppress your own natural hormones (referred to as down regulation) so that we can control the IVF cycle. When the Follicle Stimulating Hormone is introduced and the eggs start to grow it will stop them from being released naturally. This medication is continued until the trigger injection two days prior to egg collection.
Step 9: Hormone Stimulation
The FSH injection is a synthetic hormone that is self-administered, which stimulates development of ovarian follicles (think of a small sac that holds the eggs). The nurses will have shown you how to administer these.
Naturally, there will be a number of follicles that are receptive to grow every month but only one reaches maturity. By administering a higher dose of FSH than is naturally produced each month, we are able to recruit some of those follicles that wouldn't normally grow to maturity.
Step 10: Treatment Monitoring
Throughout your IVF treatment we monitor how you are responding to medication with blood tests and ultrasound scans, to measure the endometrial thickness, size and number of follicles on both ovaries. Based on this information your fertility specialist will determine when you are ready for egg collection.
Step 11: Trigger Injection
Once you have the optimum number and size of developed follicles you are ready for the trigger injection. The role of the trigger injection is to trigger the final maturation of the eggs ready for your egg collection. The nurses advise you two days before your egg collection of the exact time that you are required to administer the trigger injection. This is usually 37 hours before egg collection.
Step 12: Egg collection-day surgery
The egg collection procedure - in other words the IVF egg retrieval process - is undertaken in a day surgery unit under an anaesthetic and the procedure takes around 30 minutes. You will be at the hospital for around 4 hours and will need someone to drive or escort you home afterwards (don’t plan to work that day). The procedure is performed using an ultrasound guided probe. Attached to the ultrasound probe is a needle guide through which the fine needle passes through the vaginal wall into the ovary and draws the fluid (and egg) from the ovary. The tube containing the follicular fluid is then immediately passed to the Melbourne IVF laboratory and checked to ascertain whether it contains an egg.
On the morning of your egg collection your partner will need to provide a fresh semen (sperm) sample (unless using frozen sperm) so we can inseminate your eggs after collection.
Step 13: Fertilisation
Following egg collection, if you are having IVF treatment the egg and sperm will be placed in a dish allowing fertilisation to occur.
If you are having ICSI treatment, an embryologist will insert one single sperm directly into the egg, allowing fertilisation to occur.
Step 14: Embryo Development
The day after egg collection a scientist will contact you to discuss the number of eggs fertilised.
Your nurse will have discussed any further medication needed as well as details of your embryo transfer.
Step 15: Embryo Transfer
The embryos are returned to the woman’s uterus in a procedure called an Embryo Transfer, a simple procedure similar to a pap smear, performed by a Fertility Specialist. You will be required to have a comfortably full bladder to assist with ultrasound guidance.
No anaesthetic is usually required for the procedure, which involves a speculum being inserted into the vagina, and a narrow (2-3mm diameter) soft tube called a catheter, gently passed through the opening of the cervix.
Step 16: Embryo Freezing
Any additional embryos that are not transferred during an IVF treatment cycle, and are suitable for freezing, can be frozen for future use.
Step 17: Pregnancy blood test
A pregnancy blood test will be organised 10 days following embryo transfer.
A blood test is the only reliable pregnancy test, as urinary pregnancy test kits can provide a false reading due to the hormone medication used in IVF treatment.
Should the pregnancy test be positive, the nurses will organise an appointment with your Fertility Specialist for an ultrasound scan normally at around 6 weeks.
Once a positive pregnancy test is confirmed, you should be reassured that your pregnancy is medically no different to a naturally conceived pregnancy.
IVF medications and procedures
Medications and your IVF treatment and their treatment cycle protocols will be prescribed by your fertility specialist. For existing Melbourne IVF patients, a step-by-step guide to the different cycles, including Antagonist, Down Regulation and Flare treatment cycles, can be found in the Patient Resources section of the website.
Freezing embryos
Additional embryos not transferred during your fresh IVF cycle can be frozen for transfer at a future date. In some situations, all of your embryos are frozen (a freeze all cycle) with none being transferred as a fresh cycle. Find out more about freezing embryos and success rates with frozen embryos.
How much does IVF cost?
At Melbourne IVF, we provide access to world-class fertility treatment and advanced science with no hidden fees outside of our IVF treatment costs. We offer a range of payment options to help you manage the cost of fertility treatment.
If you have been trying to conceive for twelve months or more without success (or six months if you are over 36) we recommend a fertility assessment with a Melbourne IVF fertility specialist.
If you would like to make an appointment please call us on 1800 111 483 or complete the form below.
Meet our fertility specialists
Find out more about IVF costs
Learn more about the IVF journey with the Big Miracles docuseries